by ARC | Mar 8, 2010 | General
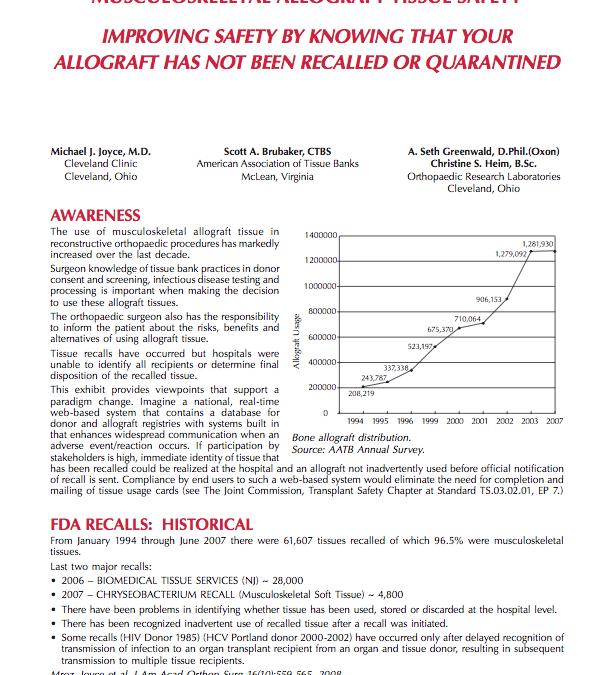
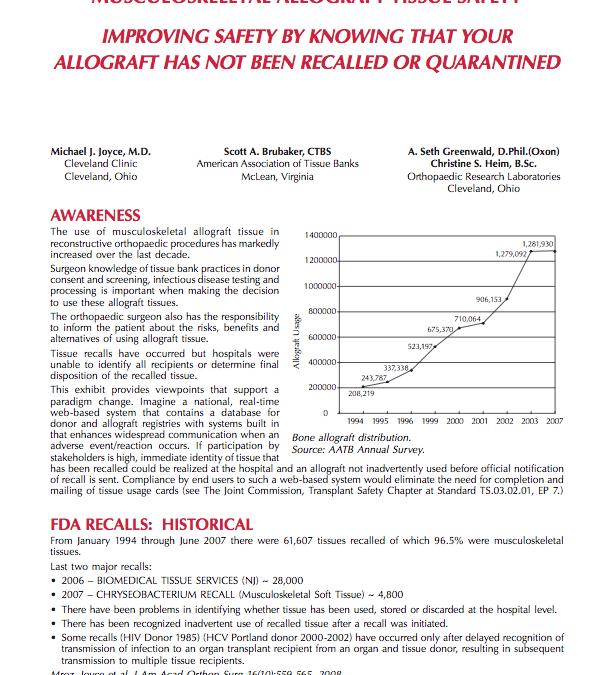
The use of musculoskeletal allograft tissue in reconstructive orthopaedic procedures has markedly increased over the last decade. Surgeon knowledge of tissue bank practices in donor consent and screening, infectious disease testing and processing is important when...
by ARC | Mar 8, 2010 | General
It is estimated that more than 500,000 bone-grafting procedures are performed annually in the United States, with approximately half of these procedures related to spine fusion. These numbers easily double on a global basis and indicate a shortage in the availability...
by ARC | Mar 8, 2010 | General
Most orthopaedic surgeons in the course of their practice will encounter and explant medical devices which have failed. Such failures may simply result from long-term in-vivo device usage, component material breakdown, technique at the time of implantation or patient...
by ARC | Mar 8, 2009 | General
More than 65 million inpatient and outpatient surgeries are done each year at U.S. hospitals. The Centers for Disease Control and Prevention (CDC) estimate that the rates of surgical site infection (SSI) range from 2% – 3% of uninfected cases – actual...

by ARC | Mar 8, 2009 | General
It is estimated that more than 500,000 bone-grafting procedures are performed annually in the United States, with approximately half of these procedures related to spine fusion. These numbers easily double on a global basis and indicate a shortage in the availability...
by ARC | Mar 8, 2009 | General
Most orthopaedic surgeons in the course of their practice will encounter and explant medical devices which have failed. Such failures may simply result from long-term in-vivo device usage, component material breakdown, technique at the time of implantation or patient...